Home | FAQs
The Centers for Medicare & Medicaid Services (CMS) are working to improve care coordination for Medicare beneficiaries. As part of that effort, CMS established a non-face-to-face chronic care management (CCM) payment reform plan for providers that began January 1, 2015. CMS uses CPT Code 99490 for providers to bill 20 minutes of non-face-to-face care coordination services for Medicare patients who have multiple chronic conditions.
The CCM payment represents new revenue that can be as high as $42.60 per patient per month depending on your geographic area. That is huge revenue for doing work that you may not be currently getting reimbursed to do. Long term, initiatives like the CCM payment program are designed to not only provide additional revenue to your practice but also help you ease into the emerging value-based care models. You will have an opportunity to gain experience in value-based care and patient-facing programs while your patients will benefit from remote monitoring and better care. coordination
All types of primary care physicians and specialists, advanced practice, registered nurses, physicians’ assistants, clinical nurse specialists and certified nurse midwives can bill Medicare for CCM. Limited-license practitioners like clinical psychologists and social workers are not eligible as well as non-physician practitioners. Starting January 1, 2016, FQHCs and RHCs became eligible to participate in the program.
No. CMS will only pay for one CCM claim per beneficiary per calendar month. If there are competing claims, CMS will most likely pay the one that is the most recent and has valid written consent from the patient to participate in the program.
Medicare patients with two or more chronic diseases that are expected to be present for at least 12 months or until death of the patient. These chronic diseases put the patient at significant risk of death, acute exacerbation/decompensation or functional decline. CMS hasn’t put out a specific list of chronic diseases because it intends for CCM services to be broadly available. CMS has a chronic conditions data warehouse that may be found at https://www.ccwdata.org/web/guest/home. This warehouse lists about 60 specific chronic conditions that would certainly fit the CCM eligibility profile..
Visit the ChronicCareIQ revenue calculator to calculate potential revenue based on your number of eligible program patients and your monthly CCM payment. There are several factors that determine your revenue but on average, providers can expect to add between $45,000 and $180,000, assuming 100% of your unique patients are covered by traditional reimbursement. Your revenue potential may be less or greater than this estimate depending on the number of eligible patients you have and how many are willing to participate in the program.
You may realize additional revenue by growing your patient numbers when other patients see the benefits provided by the CCM program. One of the biggest benefits of the CCM program is helping you transition to value-based reimbursement from fee-for-service. The CCM program also helps you improve the critical internal processes necessary to provide population health management. Instead of being at financial risk as you go to value-based payments, you are getting fee-for-service payments that support these activities.
No. CMS did build the CCM program around the principles of PCMH and did think about requiring practices to be recognized as PCMHs to get this payment but the Final Rule did not require it. However, becoming a PCMH certainly positions your practice to successfully provide CCM and many payers do offer additional incentives for being recognized as a PCMH.
Yes, there are four services that you will not be able to bill for in the same month as CCM with one exception:
The exception to these four situations concerns TCM. The same practitioner may bill for both TCM and CCM in the same calendar month for the same beneficiary if the 30-day post-discharge service period for TCM concludes before the end of that calendar month and you have provided at least 20 minutes of CCM services between the time TCM ended and the last day of that month.
ChronicCareIQ provides a comprehensive packet of information that will guide you step-by-step through setting up your program. This packet of information provides all the materials you will need to sign up patients for CCM.
The first step in beginning the CCM program is to identify all of your Medicare patients who have two or more chronic diseases that fit the eligibility requirements for this program. Once you have this list, you should schedule a face-to-face appointment with each of these patients. For example, you could inform patients about the program during a wellness check, annual physical or regularly scheduled lab. You can’t bill CCM for these types of face-to-face visits but your regular office visit fees will apply. Use the information that ChronicCareIQ provides to explain the program to your patients.
To obtain patient consent you must:
In order to provide CCM services, you will need to make sure you have an EHR that was certified to either the 2011 or 2014 certification criteria. You must also have the capacity to create a patient-centered care plan based on a comprehensive assessment of the patient. Your EHR must be capable of capturing care plan information and make it available 24/7 to all of the practice’s clinicians involved in CCM services. You must also be able to electronically share this care plan information (cannot be through a fax) with other practitioners who may provide care to the patient.
More than likely, you are already providing 24/7 access and continuity of care by providing your patients with information on how they can contact their provider if they have urgent chronic care needs. Practices typically provide access after office hours by having a number the patient can call to get in touch with their provider or by having a physician on call. 24/7 communication with providers can be by phone, internet (email, text and portals) or other non-face-to-face means of consultation.
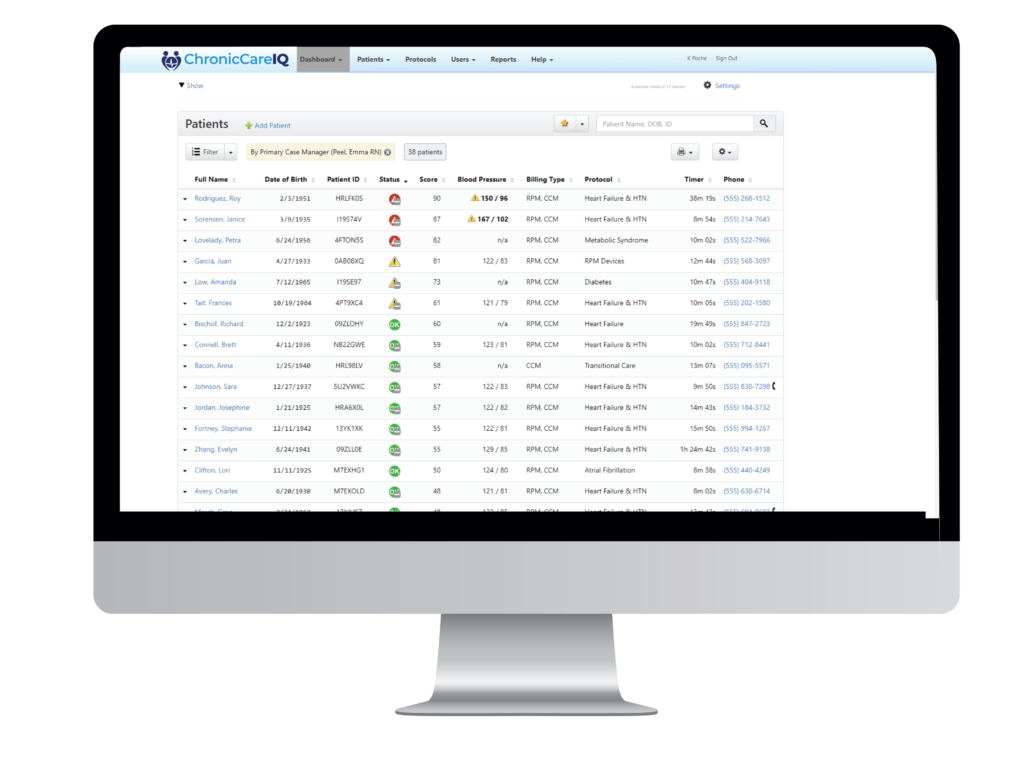
The ChronicCareIQ application and dashboard provides your practice with detailed accounting of the time you spend each month providing your eligible patients with the CCM non-face-to-face services. The application includes documentation of the staff member providing the services and details on how the time was spent. It also provides access to your comprehensive care plan and tracks the patient’s adherence to their care plan and any functional deficits that may occur during the month. ChronicCareIQ provides comprehensive audit trail and billing information that may be imported into your practice management/billing system. Any non-face-to-face actions on behalf of the patient such as consultations with other providers, filling prescriptions, reviewing patient records, etc. may also be recorded in the application to count towards the required 20 minutes per month.
ChronicCareIQ’s application provides a streamlined workflow process that automates time tracking for the CCM program. The dashboard allows your staff to easily monitor all of your CCM patients by provider. You can use the lowest licensed clinical staff, such as an MA or LPN, to monitor CCM services and triage patients who may need to be called or come in for a visit. The ChronicCareIQ dashboard shows whether the patient has entered the answers for their planned questions to monitor their conditions. Your staff can quickly see at a glance if the patient is in compliance with their care plan. The practice can develop protocols and processes for how to triage patients on the CCM program.
You should also recognize these CCM services are most likely already being provided to the patient by your practice but you are not getting paid for them!
According to Pew Research, 64% of Americans own some type of smartphone, up from 35% in the spring of 2011. Pew Research also says that Americans 65 and older who own smartphones say having one is a liberating experience. Even though only about 29% of adults ages 65 and older own smartphones, a much higher majority of their caretakers do own them. Many seniors also have a tablet such as an iPad or some type of Android tablet device. In 2014, older adults indicated they were on the internet and more than half of online seniors indicated they used Facebook. Some 56% of online adults 65 and older do so, up from 45% a year ago. Even though older Americans may not own a smartphone now, the likelihood of them getting one is very high as their usage has increased by 8 percentage points since 2014.
If your patient doesn’t have a smartphone, ask if they have a tablet or desktop computer, or if their caregiver has a smartphone. If they simply do not have the technology to use the application, a member of your staff can call them and enter their information into the dashboard to comply with the program.
ChronicCareIQ will train your staff during implementation on how to set the application up on the patient’s/caregiver’s device. Set up typically takes less than an hour and can be done during a patient’s regularly scheduled visit.
The EHR was not designed to track time or monitor how long you spend with the patient. You can use the EHR to identify your eligible patients, tag them as participants and document their care and progress in the medical record.
Using a spreadsheet to track the CCM program is time intensive for your staff which means they have less time to spend with the patient. ChronicCareIQ automates the whole non-face-to-face encounter and workflow making it easier, efficient and effective for your staff to manage. Also, CMS requires a comprehensive documentation of time spent with the patient and may audit your program. The ChronicCareIQ application provides extensive documentation for audits that will save you time and money if you are audited.
See for yourself how we can help you grow without adding more resources or risk.
Now is the time to explore a better care management solution that gives you confidence to grow your practice while giving patients confidence in managing their complex conditions.
© 2024 ChronicCareIQ, All rights reserved