With ChronicCareIQ, your practice can perform chronic care management (CCM) confidently and profitably without adding staff or a third-party call center.
Award-winning technology solution that proactively engages eligible patients and obtains updates including vitals and current symptoms.
A red-yellow-green dashboard analyzes patients’ responses and alerts staff to those trending poorly or exceeding clinical thresholds so you can intervene sooner and provide higher quality care.
ChronicCareIQ also integrates with your EHR and phone system to ensure all eligible activities and patient contact points are automatically captured, timestamped and documented with the appropriate CCM reimbursement codes.
The result? Better patient outcomes, better documentation, and optimized reimbursements.
“If my patients experience changes in their symptoms or report readings that fall outside of our clinical thresholds, I know immediately through my ChronicCareIQ dashboard. I feel that I'm able to do my job much more efficiently and successfully by having a single view into all of my patients in one simple dashboard.”
Donna Hardy, Chronic Care Coordinator, Birmingham Heart Clinic
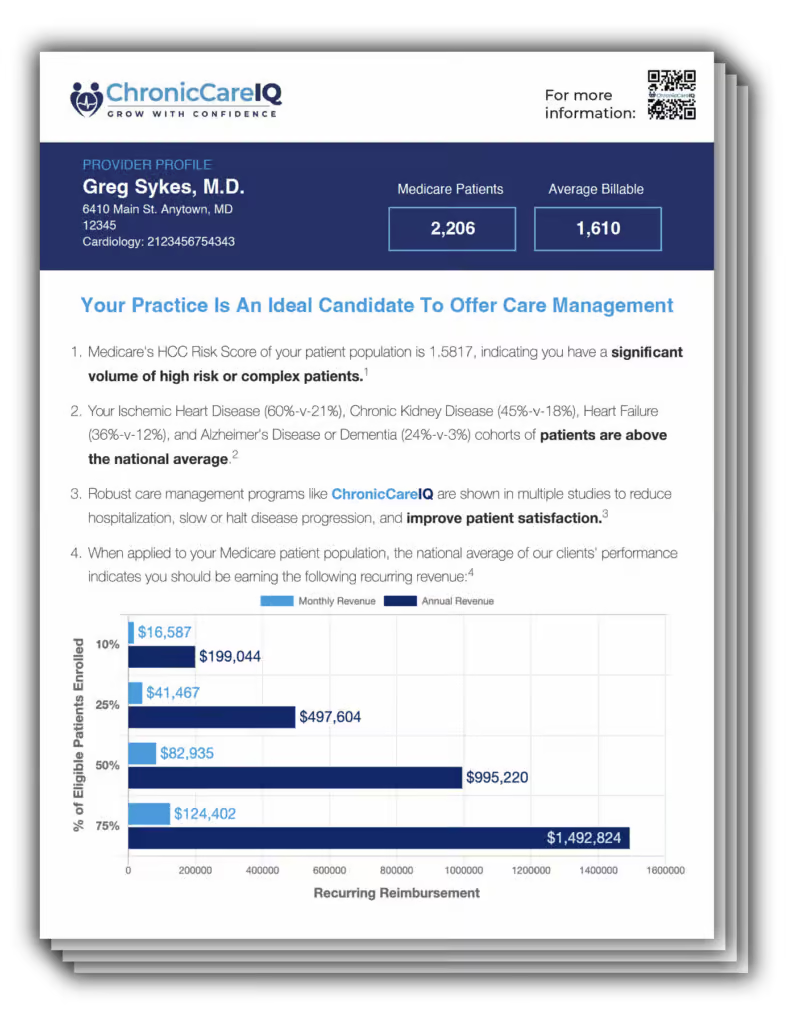
Use our Reimbursement Analysis Tool and unlock your potential for increased revenue.
Discover your potential for increased revenue with chronic care management by entering your NPI number in our Reimbursement Analysis Tool below. The personalized provider profile analyzes your patient population’s chronic conditions and provides monthly reimbursement estimates tailored to you.
Once patients are enrolled in your care management program, the system begins to proactively engage with them according to the clinical protocols you set for their specific chronic conditions. Engagement comes in the form of a series of simple questions that patients respond to – either on their phone, tablet, or personal computer. And 87% of those who start are still engaged one year later.
As your team provides care and supportive services, such as phone calls, coordinating medication refills, patient education, and care coordination with specialists and testing centers, the system recognizes those interactions and automatically captures and timestamps each activity for reimbursement. Each eligible activity is then assigned the appropriate care management program codes. There is no need for staff to manually provide documentation or follow reimbursement guidelines for hitting certain thresholds – the system does the work for them.
Your clinical team members simply review their red-yellow-green dashboards to know which patients are trending in the wrong direction or those who have exceeded pre-set clinical thresholds. They can drill down to the details of each patient, review recent interactions and see the latest data coming in from patients and/or monitoring devices. This gives them a complete picture of the patient in real-time so they can make more informed decisions about what needs to happen for each patient. Earlier intervention not only improves outcomes and patient satisfaction, it also makes complex patients easier to care for and reduces the burden on staff.
Your back-office staff has access to reports that show which clinical activities were performed on which patients so preparing claims for reimbursement is simple. The system not only quantifies but also qualifies where the time was spent, so you know exactly what to bill for each patient. This helps protect your practice from over or under billing without appropriate documentation. All the pieces come together.
Everything you need to know about maximizing CPT billing
Want to know the ins and outs of new opportunities to boost reimbursements for 2025? Which CPT codes are extensions of others, and which aren’t combinable? How about which programs are affected by the recent elimination of time-based thresholds?
It’s all here in ChronicCareIQ’s comprehensive CPT Billing Code resource guide.